Sciatica Exercises for Pain Relief and Recovery
If you've ever experienced a sharp, shooting pain that travels from your lower back down through your leg, you're likely familiar with sciatica. This nerve-related condition affects countless people, causing anything from mild discomfort to severe pain that disrupts sleep, work, and daily activities. Unlike general back pain, sciatica has a distinctive radiating quality that follows the path of the sciatic nerve. Fortunately, with the right approach, including targeted exercises, appropriate treatment, and supportive therapies, most people can manage their symptoms effectively and regain their quality of life.
Understanding Sciatica: Causes and Symptoms
What is Sciatica?
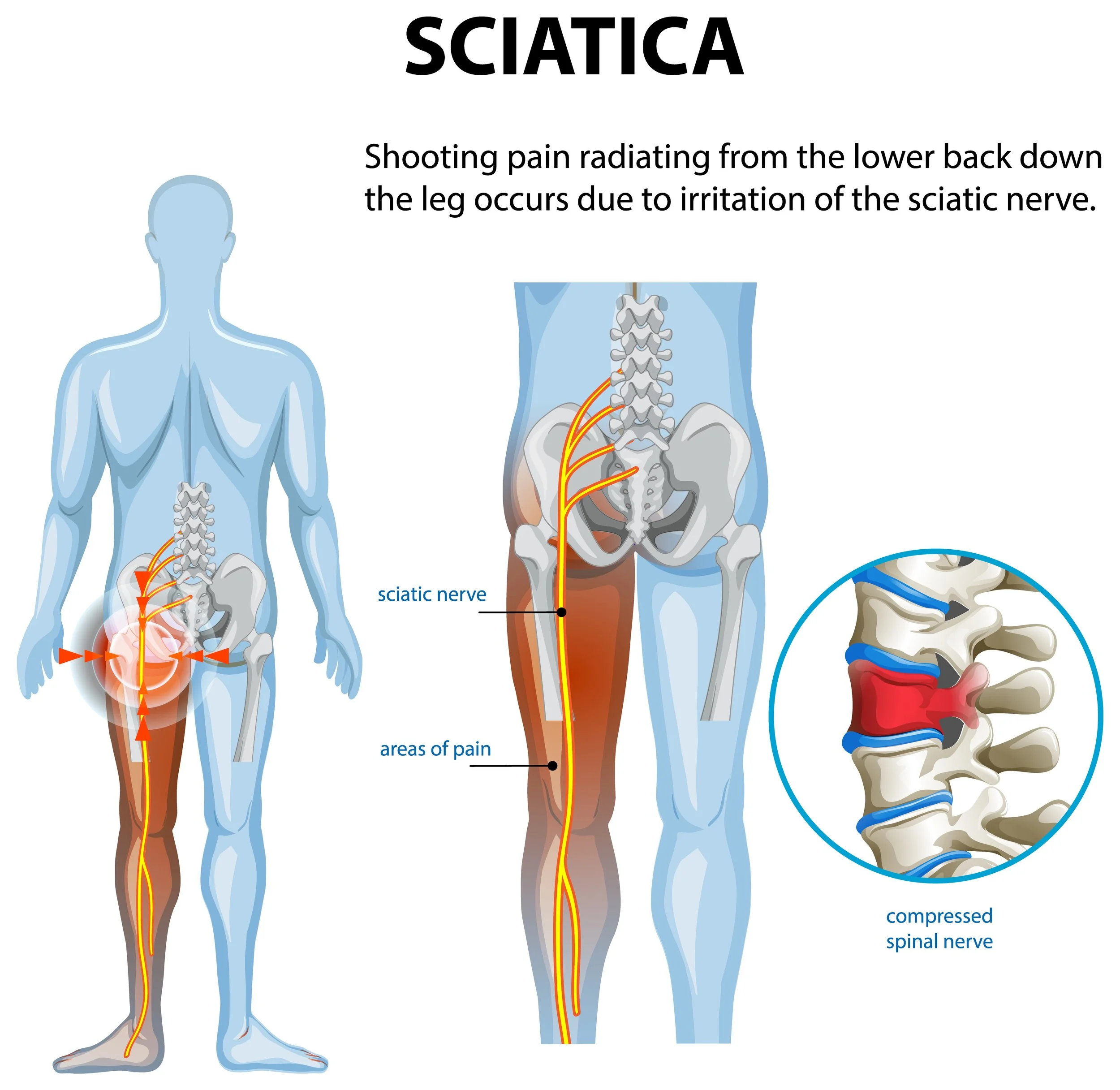
Sciatica refers to pain that travels along the path of the sciatic nerve, which branches from your lower back through your hips and buttocks and down each leg. Rather than being a condition itself, sciatica is a symptom of an underlying problem affecting the sciatic nerve, the longest and thickest nerve in the human body. The pain typically affects only one side of the body and can range from a mild ache to a sharp, burning sensation or excruciating discomfort.
Types of Sciatica
Sciatica is generally classified into two types:
Acute sciatica develops suddenly and typically lasts from a few days to several weeks. It often results from a specific injury or movement and usually responds well to conservative treatment.
Chronic sciatica persists for three months or longer and may require more comprehensive management strategies. This type often involves persistent nerve irritation or underlying structural problems.
Common Symptoms
Sciatica presents with distinctive symptoms that help distinguish it from other types of back pain:
Sharp, shooting pain that radiates from the lower back through the buttock and down the back of the leg
Numbness or tingling sensation in the leg or foot
Muscle weakness in the affected leg or foot
Pain that worsens with prolonged sitting, standing, or sudden movements
A burning or electric shock-like sensation
Difficulty moving the leg or foot
Pain that typically affects only one side of the body
The intensity can vary significantly, from occasional mild discomfort to constant, debilitating pain that interferes with daily activities.
Causes and Risk Factors
Understanding what causes sciatica can help in both treatment and prevention. The most common causes include:
Primary Causes:
Herniated or bulging disc is the most frequent cause, occurring when the soft cushion between vertebrae pushes out and compresses the sciatic nerve
Spinal stenosis involves the narrowing of the spinal canal, putting pressure on nerves
Piriformis syndrome occurs when the piriformis muscle in the buttocks irritates the sciatic nerve
Degenerative disc disease causes wear and tear on spinal discs over time
Spondylolisthesis happens when one vertebra slips forward over another
Spinal injuries or tumours (less common but serious)
Risk Factors:
Age-related changes in the spine, particularly after 40
Obesity, which increases stress on the spine
Prolonged sitting or a sedentary lifestyle
Occupations requiring heavy lifting, twisting, or driving for long periods
Diabetes, which increases the risk of nerve damage
Poor posture and improper lifting techniques
How to Treat Sciatica
Treating sciatica effectively requires a multifaceted approach tailored to the severity and underlying cause. Most cases improve with conservative treatments within a few weeks.
Conservative Treatments:
Initial treatment typically involves self-care measures and non-invasive therapies. Apply ice packs to the affected area for the first 48-72 hours to reduce inflammation, then switch to heat therapy to relax muscles and improve blood flow. Over-the-counter pain relievers like ibuprofen or paracetamol can help manage discomfort. Maintaining gentle activity is crucial, whilst complete bed rest was once recommended, staying active (within pain limits) promotes faster recovery.
Medical Interventions:
When conservative measures aren't sufficient, medical treatments may include:
Prescription medications such as muscle relaxants, anti-inflammatories, or nerve pain medications
Epidural steroid injections to reduce inflammation around the affected nerve root
Physical therapy with personalised exercise programmes and manual therapy techniques
Chiropractic care for spinal adjustments and alignment
Acupuncture which may provide relief for some patients
Surgical Options:
Surgery is typically reserved for severe cases where conservative treatments have failed after several months, or when there's progressive weakness or loss of bladder/bowel control. Procedures may include microdiscectomy to remove herniated disc material or laminectomy to relieve pressure on the nerve.
Lifestyle Modifications:
Long-term management involves maintaining a healthy weight, practising good posture, using proper lifting techniques, taking regular breaks from prolonged sitting, and incorporating regular exercise into your routine.
Sciatica Exercises
Targeted exercises are one of the most effective ways to relieve sciatica pain and prevent recurrence. They help stretch tight muscles, strengthen supporting structures, and improve flexibility. Always consult your healthcare provider before starting any exercise programme, especially during acute pain.
Stretching Exercises for Sciatica to Improve Flexibility
Stretching helps relieve pressure on the sciatic nerve and reduces muscle tension:
Knee-to-chest stretch: Lie on your back, gently pull one knee towards your chest, hold for 20-30 seconds, then switch legs. This stretches the lower back and glutes.
Piriformis stretch: Lie on your back with knees bent. Cross the affected leg over the other knee, then pull the lower leg towards your chest. Hold for 30 seconds to release tension in the piriformis muscle.
Seated spinal twist: Sit with legs extended, cross one leg over the other, and gently twist towards the bent knee. This mobilises the spine and stretches the outer hip.
Child's pose: Kneel on the floor, sit back on your heels, and stretch your arms forward on the ground. This gently stretches the lower back and promotes relaxation.
Standing hamstring stretch: Place one foot on a low step or chair, keep your leg straight, and lean forward slightly. Tight hamstrings often contribute to sciatica.
Figure 4 stretch: Lie on your back, cross one ankle over the opposite knee, and pull the uncrossed leg towards your chest. This deeply stretches the hip and glute muscles.
Strengthening Exercises to Support the Lower Back and Hips
Building strength in your core and lower body provides better support for the spine:
Pelvic tilts: Lie on your back with knees bent, flatten your lower back against the floor by tightening your abdominal muscles. Hold for 5 seconds, then release. This strengthens deep core muscles.
Bridges: Lie on your back with knees bent, lift your hips towards the ceiling, squeeze your glutes, and hold for 5 seconds. This strengthens the glutes, hamstrings, and lower back.
Bird-dog: Start on hands and knees, extend one arm forward and the opposite leg back, hold for 5 seconds, then switch. This builds core stability and balance.
Partial crunches: Lie on your back with knees bent, hands behind your head, and lift your shoulders slightly off the ground. This strengthens abdominal muscles without straining the back.
Wall sits: Stand with your back against a wall, slide down into a sitting position, and hold for 10-30 seconds. This strengthens the quadriceps and glutes.
Clamshells: Lie on your side with knees bent, keep feet together, and lift the top knee whilst keeping hips stable. This targets hip abductors and improves pelvic stability.
Precautions and Tips for Safe Sciatica Exercise Practice
To maximise benefits and minimise risk:
Start gradually: Begin with gentle movements and slowly increase intensity as your pain improves
Listen to your body: Some discomfort is normal, but stop if you experience sharp, shooting pain
Maintain proper form: Poor technique can worsen symptoms, so consider working with a physiotherapist initially
Breathe steadily: Avoid holding your breath during exercises
Be consistent: Aim to perform exercises 2-3 times daily for best results
Warm up first: Gentle walking or light activity prepares muscles for stretching
Avoid aggravating movements: Skip exercises that significantly increase pain
Progress slowly: Gradually increase repetitions and duration over weeks
Combine with other treatments: Exercises work best as part of a comprehensive treatment plan
Massage for Sciatica
Massage therapy can be a valuable component of sciatica treatment, offering pain relief and promoting healing when performed correctly.
Benefits of Massage
Therapeutic massage helps reduce muscle tension, improve blood circulation, release trigger points, promote relaxation, and reduce stress-related muscle tightness. By targeting specific muscles that may be compressing or irritating the sciatic nerve, massage can provide significant relief.
Effective Massage Techniques
Deep tissue massage targets deeper muscle layers to release chronic tension and break up scar tissue
Trigger point therapy focuses on specific tight knots in muscles that may be contributing to nerve compression
Myofascial release addresses the connective tissue surrounding muscles, improving mobility
Swedish massage uses gentle, flowing strokes to promote relaxation and reduce overall muscle tension
Target Areas
Focus massage on the lower back, glutes (especially the piriformis muscle), hamstrings, and hip flexors. These areas commonly harbour tension that contributes to sciatica symptoms.
Self-Massage Techniques
You can also perform self-massage at home:
Use a tennis ball or foam roller against a wall to massage the glutes and lower back
Roll a massage ball under your hamstrings whilst seated
Apply gentle pressure with your thumbs along tight muscles
Use a handheld massager on accessible areas
Professional Massage Considerations:
When seeking professional massage therapy, choose a qualified remedial or sports massage therapist experienced in treating sciatica. Communicate clearly about your symptoms and pain levels, and avoid massage during acute inflammation or if you have certain medical conditions. Always consult your healthcare provider before starting massage therapy, especially if you have severe symptoms.
Important Precautions:
Massage should complement, not replace, other treatments. Avoid deep pressure directly on the spine, and stop immediately if the massage significantly increases pain or causes numbness. If symptoms worsen after a massage, consult your healthcare provider.